Duration of Insulin Action
Adjusting Insulin (Pump): duration of insulin action (DIA)
If you pump your insulin, you have likely heard of DIA, or Duration of Insulin. But what exactly does DIA represent? Here we go into detail about what it is, how it's different from ISF, how the DIA setting affects calculation of insulin on board, and how to assess how long insulin lasts in your child's body (and therefore, how to program an accurate DIA pump setting).
Before Reading This Article...
If you have not done so already, we recommend that you read the following WaltzingTheDragon.ca pages on insulin adjustment for pumps as background for the information that follows:
A Basal-Bolus Approach to Insulin Pump Therapy
How Insulin Action Impacts Blood Glucose in an Insulin Pump Program
Insulin Adjustment for Pumps: an Overview
Testing and Tweaking Basal Rates in an Insulin Pump Program
Adjusting Insulin-to-Carbohydrate Ratios with an Insulin Pump
Adjusting Insulin Sensitivity Factor (ISF) in an Insulin Pump
What is Duration of Insulin Action?
Duration of Insulin Action (DIA)
= the length of time (after a dose of insulin is given) during which that insulin is still active.
How long does a given dose of rapid-acting insulin work (to lower blood glucose and/or to use food for energy)? When asking this question, we’ve received a range of answers, from 3 hours up to 5-6 hours. This variation is based partly on individual differences: different people metabolize (“use up”) insulin at different rates. Duration of insulin action may also vary between different brands of insulin (here in Canada, that would include Humalog®, NovoRapid®, Apidra® and Fiasp®). Therefore, it is important to check whether the current IOB/DIA setting programmed into your child’s pump is appropriate, as the bolus calculator in the pump uses this programmed number to calculate whether or not active insulin remains at a certain point in time following a bolus (which will, in turn, affect the dosing suggestions for correcting high BG, and, in some cases, to cover food carbs).
The Duration of Insulin Action setting that you program into your child's pump will affect calculations of the active insulin, or Insulin on Board. If you tell the pump that the insulin will last for 3 hours, then at the end of that time the pump will tell you that there's zero active insulin remaining (and will therefore recommend a correction for an above-target BG at the 3-hour point). Compare that to telling the pump that the insulin will last for 6 hours: at the 3 hour point, the pump will tell you that there is still 50% of the original bolus remaining as active insulin, and will recommend a much lower correction, or possibly a zero correction, for an above-target BG at the 3-hour point. For this reason, programming in an accurate Duration of Insulin setting is an important part of avoiding blood glucose swings.
What’s the Difference between “Duration of Insulin Action” and “Insulin Sensitivity Factor”?
Duration of Insulin Action (DIA) is a measure of how long insulin works to lower BG (in hours).
Insulin Sensitivity Factor (ISF) is a measure of how much BG is lowered by 1 unit of insulin (in mmol/L).
For example, if a correction dose of rapid-acting insulin lowers blood glucose from 14.5 mmol/L to 7.5 mmol/L between 10 pm and 2 am, and then was steady (did not drop further) after 2 am, then:
Insulin Sensitivity Factor (ISF) is related to the BG drop of 7 points (and would be expressed as 1:7), while
Duration of Insulin Action (DIA) refers to the time period of 4 hours that it took to do so.
Initial DIA Settings
How Do I Know What Number to Program Into the Pump?
Your child’s diabetes health care team should advise you of an initial Duration of Insulin setting to program into the pump. In talking with other families, it seems that many individuals use 3 hours, 3.5 hours, or 4 hours as the DIA setting. If your child currently uses a similar setting, then that is consistent with many other pump users. If your child uses a shorter or longer setting, that may still be the best setting for him, even though it may not match the setting used by many pump users – every body has individual needs. If you would like to check whether that programmed setting is the most appropriate setting for your child at this time, you may test the current setting as outlined below.
Assessing Current DIA Settings (Pump)
If you often find that, even after the pump says you have no active insulin left, blood sugar continues to drop (assuming you have already confirmed the basal rates, and have not just engaged in physical activity), then the Duration of Insulin Action may be set for too short of a time period. For example, you have programmed the pump for a DIA of 4 hours, but your insulin is actually lasting 5 hours. Conversely, if the insulin consistently does not seem to last as long as you thought, and blood glucose is rising when the pump says that you still have active insulin remaining, (again, assuming you have already confirmed the basal rates, are not under stress, and did not eat high fat or low glycemic foods recently), then the current Duration of Insulin Action may be set for too long of a time period. For example, you have programmed the pump for a DIA of 5 hours, but your insulin is actually lasting only 4 hours. In either case, a consistent pattern either way may indicate that you need to adjust the pump’s Duration of Insulin Action setting .
Conditions for Testing DIA
- no active insulin already working (no bolus in the last 4 hours)
- not eat/drink during the test period and for 4 hours before the test period begins.
- Only healthy meal/snack before the test period, avoiding fatty foods and restaurant/takeout food.
- typical exercise levels before the test period. (Light to moderate physical activity is okay, if your child usually does so at that time of day)
- not have had any lows in the last 12 hours.
- not be sick.
- not be at the beginning of or just prior to a menstrual cycle.
- not disconnect or suspend the pump during the pre-test or during the testing period.
DIA Testing Process & Results
When BG is above target (and the above conditions are met), give a correction dose of insulin and see how long it takes for BG readings to STOP DROPPING. You are not primarily attending to how low BG drops, which would be a test of the current ISF setting (although this test can be done at the same time as a DIA/IOB test). Instead you are noting how long it takes the insulin to stop working; that is, how long before BG readings level out.
For example:
Your child’s BG was 14.5 at 10pm, the last bolus was given at 5:30pm and supper was finished by 6:00pm. The usual correction dose of rapid-acting insulin was delivered at 10:00pm. BG was checked at 2, 3, 4, and 5hrs later, with the following results:
12:00am: 12.1
1:00am: 10.5
2:00am: 9.5
3:00am: 9.6
BG readings dropped from 10pm to 2am (for 4 hours), then did not drop further after that. Therefore, it makes sense to set the DIA setting at 4 hours. If your child’s pump allows IOB to be set in half hour increments, you could check BG at half-hour points after the 3-hour mark, to see if your child’s individual IOB setting is actually 3.5 hours. In this case, in the context of the above example, if the 1:30am BG reading was 9.5, then the insulin actually stopped lowering BG at 1:30 (not 2:00am), so you may choose to set IOB at 3.5 hours, rather than 4 hours. If the 1:30am reading was 10.2, then BG did not stop dropping until 2 am, so you may choose to set DIA/IOB at 4 hours.
What Do the Test Results Also Tell Me About ISF?
As explained above, Duration of Insulin Action (DIA, or IOB) is a measure of how long insulin continues to lower BG, while Insulin Sensitivity Factor (ISF) is a measure of how much the BG is lowered (by 1 unit of insulin).
In analyzing the test results above, it is important to note: if your child’s target BG during this time is 7.0 mmol/L, then this correction dose of insulin did not reduce BG enough (not enough insulin was given), as the lowest BG was 9.5 mmol/L, which is above target. This is related to the ISF setting; it is NOT related to the IOB setting.
However, if your child’s target BG during this time period is 9.5 (or 9.0, for that matter), then the insulin dose given worked to lower BG to the target, thus this test would have verified the current ISF setting.
More about adjusting Insulin Sensitivity Factor (ISF):
Additional Notes:
- Accurate results depend upon previous confirmation of basal rates during this time period. If basal rates are set too high, BG may continue falling even after the bolus is “used up” (due to basal insulin, rather than due to the correction dose which you are attempting to test). This will confound the test results. Therefore, basal rates need to be confirmed before testing DIA.
- Unlike basal, I:C and ISF settings which change often as your child grows and changes, DIA seems to be a more stable construct. You may only have to do this test very occasionally, as the results are less likely to change significantly over time.
- We could not find any scientific evidence suggesting either that you need to change the DIA setting when you change brands of rapid-acting insulin, or that you can count on things staying the same between different brands. If unsure, you may want to re-check DIA after a change in insulin. Fiasp® is the one fast-acting insulin that may require you to alter previous DIA settings when you start using it, as it was developed specifically to act faster, and to have a shorter “tail”.
- Because of the required conditions, this test may most easily be carried out overnight. Night-time results are likely to apply to daytime DIA also.
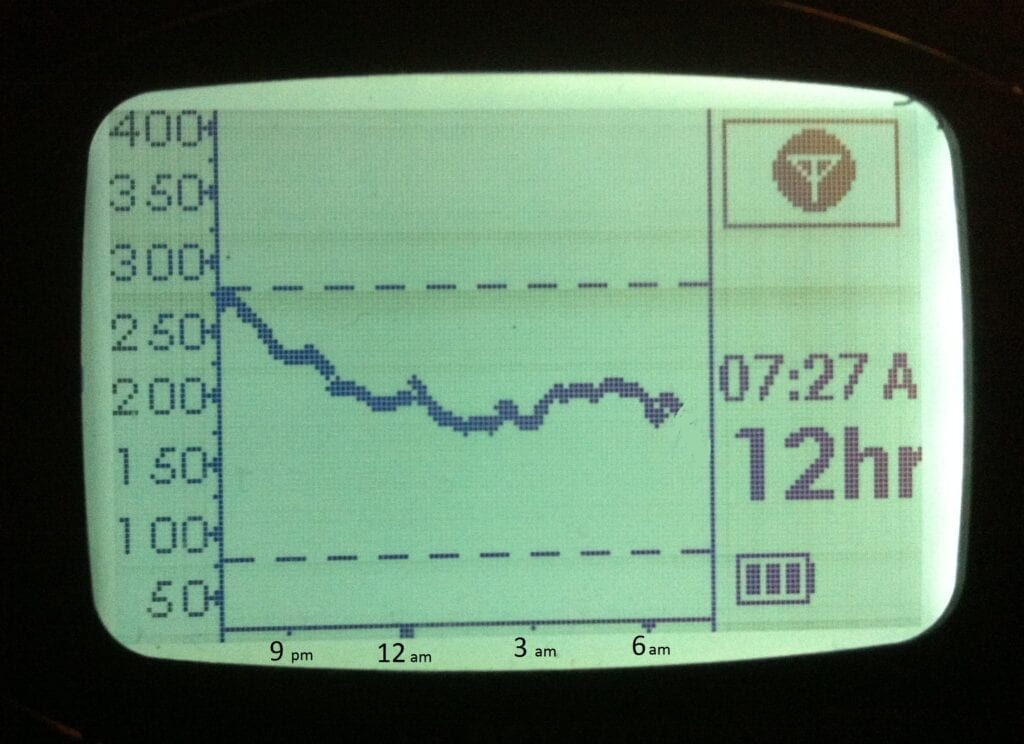
- Using a Continuous Glucose Monitor (CGM, or glucose sensor) to conduct this test means that you will not have to wake up every hour or half-hour to check BG. Instead, you may choose to review the CGM trace in the morning, noting what time (that is, how many hours after the delivery of the correction bolus) the graph leveled out. A CGM provides a nice visual representation of the results, which for those visual-processors in the crowd, may be more easily interpreted.
In this example CGM trace, blood glucose drops from the time the correction bolus was delivered at 7:30 pm (the start of the graph) until about 12 am (4.5 hours), then levels out for the following 6 hours. This trace suggests that a DIA setting of 4.5 hours may be appropriate.
Tip from the Trenches
We originally set my son’s IOB setting at 3.5 hours. When we changed it to 4 hours, the reduction in BG swings was noticeable. It seems that this was happening: when the pump calculated a correction dose at 3.5 hours, it did so assuming that there was no insulin still acting. But, apparently, my son’s body takes a little longer to use up his insulin, so at 3.5 hours, there WAS still active insulin remaining. As a result, when we gave a correction dose we were over-correcting, resulting in below-target BG’s later. When we started taking this unused insulin into account, we empowered the pump to calculate a more appropriate dose. (It is possible that the lows were caused by an inappropriate ISF setting, rather than IOB. How did we guess that the IOB, rather than the ISF, setting needed adjusting? When we gave a correction dose with more than 4 hours since the last insulin dose, our correction worked, we did not see a trend of lows. This suggests that ISF was set correctly, which left the IOB setting to test and adjust.)
~Michelle
The above information was reviewed for content accuracy by clinical staff of the Alberta Children’s Hospital Diabetes Clinic.
SHARE THIS ARTICLE